Basic Facts of Hereditary Cancers
Cancer has become such a common disease that it is no surprise that many families have more than one family member who have had cancer. Sometimes, certain types of cancer seem to run in some families. Very often, it may due to certain risk factors shared by family members for example lifestyle and environmental factors such as smoking and high fat content diet that links to obesity, tend to be common traits in families and can increase cancer risks.
But in some cases the cancer is caused by an abnormal gene that is being passed along from generation to generation. Although this is often referred to as inherited cancer, what is inherited is the abnormal gene that can lead to cancer, not the cancer itself. Only about 5% to 10% of all cancers result directly from gene defects (called mutations) inherited from a parent. Hereditary Breast, Ovarian, and Prostate Cancer is one of the common types.
Hereditary Breast, Ovarian, and Prostate Cancer
Among all breast cancer patients, hereditary cancers constitute 10-15%.
When breast cancer occurs due to a hereditary cause, women tend to have breast cancer at a younger age (usually pre-menopausal). The most common gene mutations are in the BRCA 1 and BRCA 2 gene.
Mutations of BRCA 1 and BRCA 2 genes are one of the most important factors for developing hereditary breast and ovarian cancers. The two genes are inherited and cannot be changed by modifying your lifestyle, thus the risks cannot be overlooked.
Lifetime risk of breast cancer:
- in women: 10 times higher than the population risk
- in men: 60 times higher than the population risk
Lifetime risk of ovarian cancer:
- 50 times more than the population risk.
Lifetime risk of prostate cancer:
- 4.5 times more than the population risk.
It may also relate to other types of cancers such as pancreas, stomach, colon, laryngeal, bile duct, and melanoma.
Who should be tested?
The following personal and family medical history may indicate an increased likelihood of having BRCA mutations:
- Early onset of breast cancer (breast cancer diagnosis before 45 and below)
- Early onset of ovarian cancer (ovarian cancer diagnosed before menopause especially)
- Multiple cases of breast cancer and related cancers (eg. Prostate cancer), especially with early onset
- Ovarian cancer (with family history of breast or ovarian cancer)
- Breast and ovarian cancer in the same woman
- Bilateral breast cancer
- Male breast cancer
- The one with breast, ovarian, and prostate cancer history in the family.
- First-degree relatives of mutated gene carrier.
- Some second-degree relatives of mutated gene carrier.
* The one who has youngest onset of related cancer in the family should be tested first
For other cancers, BRCA mutation test may be suitable if there is also a family history of breast cancer. However in certain circumstances it may be more appropriate to do genetic test to look for mutations in other genes. Our genetic counsellor will be able to give you suggestions following the genetic counselling session.
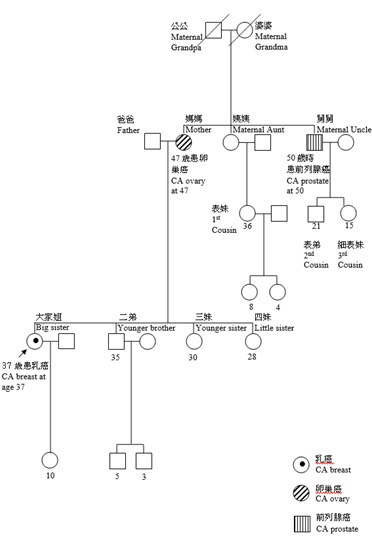
Pedigree (insert 2015 Breast Concern Action version-with graphics)
Management for High Risk Patients
Cancer surveillance for females
Although the current recommended breast cancer surveillance for women starts at age 40 and above, high risk individuals are recommended to begin a more intensive screening much earlier (at the age of 18). A monthly breast self-examination, bi-annual clinical breast examination, mammographic (to begin at the age of 25-30) and ultrasonic breast screening and magnetic resonance imaging (MRI) are recommended for high risk women (NCCN, 2015).
Cancer surveillance for males
For male carriers, periodic clinical examination of the breasts and regular screening for the prostate is necessary to prevent/detect tumour in an early stage. As prostate cancer risk was the most persistent finding for men with BRCA1 or BRCA2 germline mutation in families with cancer history, prostate specific antigen (PSA) and digital rectal examination (DRE) testing are recommended to be performed regularly, at least once a year (Berliner et al., 2013).
Prophylactic surgeries
Alternatively, individuals can opt for a more radical procedure to reduce the risk to a minimum. The removal of breasts (prophylactic mastectomy) and ovaries (prophylactic salpingo-oophorectomy) can reduce up to 90% of breast cancer incidence and 85% of ovarian cancer incidence in women with BRCA1/2 mutations. However, studies in Asia have shown that surveillance is still the most popular choice of management among Asian gene mutation carriers. The majority of high-risk females usually prefer close monitoring as mentioned with chemoprevention to lower the risk of developing breast and ovarian cancer.